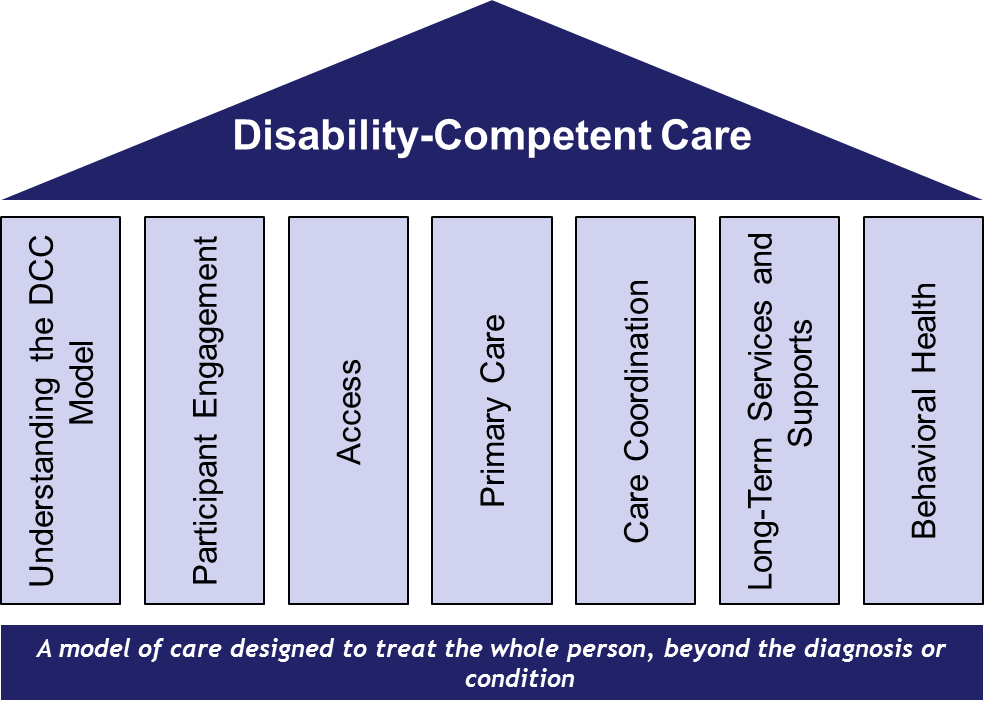
A model of care designed to treat the whole person, beyond a diagnosis or condition.
The DCC Model
Disability-competent care (DCC) is an aspirational, participant-centered model that focuses on the eventual goal of supporting individuals to achieve maximum function. The DCC model is delivered by an interdisciplinary team (IDT) whom recognizes and treats each individual as a unique person, not their diagnosis or condition. The model encourages participant direction in choices regarding their health, wellness, and life in the community. DCC responds to the participant’s physical and clinical requirements while also considering emotional, social, intellectual, and spiritual needs. Persons with disability are a diverse group with varying characteristics. Therefore, DCC requires that health care providers understand the participant’s disability experience; the clinical diagnosis of the disability; and the functional limitations that individuals with disability may experience.
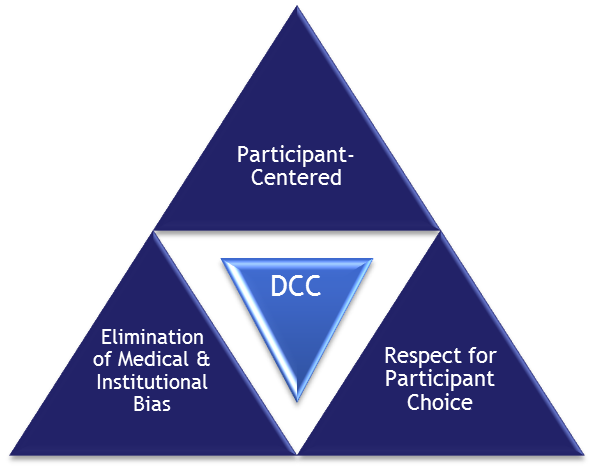
Applying the Disability-Competent Care model requires an understanding and appreciation of the three core values which are supported by seven functional area pillars.
Core Values of the Disability-Competent Care Model
The core values of the DCC model are focused on the individual needs of the participant, respect for the participant’s choices, and the elimination of medical and institutional bias. These values are intricately woven throughout the fabric of the DCC model and are key drivers in the delivery of a participant-centered care approach. A mainstay concept and a common linkage between each core value is the focus/attention to understand each participant’s unique disability and their functional impact on the participant. This truly drives home the importance placed on the participant and the model’s intent on making them the focal point.
There are three core values that form the basis of the DCC model.
A. Participant-centered approach recognizes the participants’ preferences, goals, and choices that provide the foundation for their individualized plan of care (IPC).
B. Respect for the participant’s choice and the dignity of risk, which honors and respects the participant’s choices even if they are inconsistent with health care recommendations.
C. Elimination of medical or institutional bias that may impede providers and plans from addressing the individual as a whole. Biases may include unique disabilities, limitations, and preferences for social and community participation.
Seven Pillars of the Disability-Competent Care Model
The DCC pillars are comprised of seven functional areas. Each functional area represents a standalone pillar. Together, these pillars form the foundational structure of the DCC model.
The DCC pillars provide an organizational context to the overall model and its content. Products and resources are organized based on functional area. Within each pillar, three unique stages of DCC comprehension are outlined: 1) understanding topic principles, 2) recognizing topic improvement opportunities, and 3) actualizing and refining identified topic opportunities. Each stage provides its own unique set of resources, tools, and products; providing tailored materials for the varying levels of DCC proficiency.
There are seven pillars that comprise the DCC model.
- Understanding the DCC Model and the population being served.
- Focusing on Participant Engagement and implementing participant-centered care.
- Helping participants have Access at all phases of health care delivery and community participation.
- Developing and integrating responsive Primary Care.
- Identifying key Care Coordination needs across the full spectrum of services, including transitions and leveraging community supports.
- Establishing flexible Long-Term Services and Supports (LTSS) so participants have the resources needed to function in the community.
- Integrating Behavioral Health services to help participants receive integrated care,
Disability Competence And My Organization
It is important to evaluate an organization’s current ability to meet the needs of its participants (or members) and to identify strategic opportunities for improvement. Several tools are available to assist in these efforts.
- The Disability-Competent Care Self-Assessment Tool (DCCAT) will help organizations (e.g., health plans and health systems) evaluate their current ability to meet the needs of participants with functional limitations and identify strategic opportunities for improvement.
- The Disability-Competent Care Self-paced Training Assessment Review Tool (DCC START) will help organizations understand their current inventory of DCC training materials, identify tailored areas of opportunity, and provide resources to address findings and strengthen overall training materials/curricula.